Tons of paperwork and clinical data filing are among the concerns healthcare practitioners have faced over the years. The past decade has been more about restructuring as the healthcare industry adopted technological advancements. As the narrative changed with time, so did the contemporary healthcare software architecture. With custom healthcare software development services, healthcare practitioners have infused their systems with the unprecedented need for transformation. EMR/EHR software development helps maintain records and ensure that the data stays secure, which was among the changes welcomed.
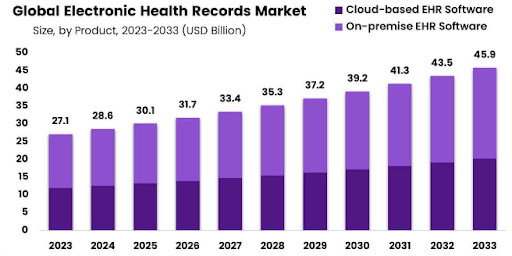
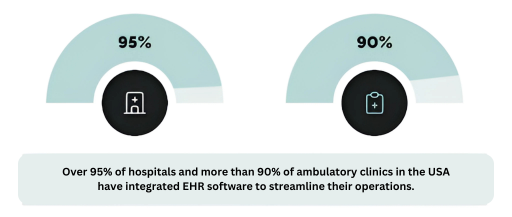
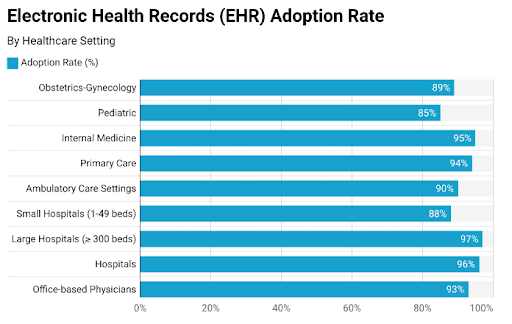
For instance, the National Coordinator for Health Information Technology’s data show that 96% of hospitals and clinics chose EMR/EHR integration into their existing systems. Such a statistic invokes the hospital’s urgency to transform. The worldwide EHR market revenue is predicted to reach $45.9 billion by 2033. This makes them look for a medical software development company with experience building EMR and EHR systems.
The digital transformation in healthcare begins with basic R&D, an analysis of the advantages, and the addition of essential EMR/EHR features. It ends with estimating the cost of implementing EHR/EMR. We present a bifurcated guide with a 360-degree analysis to steer through the healthcare businesses and practitioners.
What is EMR/EHR Software?
When we articulate an EHR software, the supplementary phrase that typically surfaces as a replacement is EMR. Often used interchangeably, there is an extensive distinction between the two: electronic health records and electronic medical records.
An electronic medical record (EMR) is a digitalized interpretation of a patient’s data reserved inside a hospital. It retains the patient’s medical and restorative history during one routine. However, electronic health records systems are designed to be transferred with labs, administration, patients themselves, and other health providers. However, they are not permitted to be disseminated beyond the clinic.
Types of EHR and EMR Systems
From a technological perspective, hospital management systems have been diversified into distinct kinds, each with distinguishable applications in the healthcare industry. As we comprehend through EHR software development, we must analyze the types of cost-effective EMR solutions to decide which ones suit your healthcare requirements.
Web Based
These web-based EHRs are available through a web browser, making them more suitable if you have numerous establishments or healthcare specialists requiring remote access.
Mobile App based
With healthcare application development, practitioners can build mobile-based EHRs that are accessible feasibly through smartphones and tablets by users and patients.
Cloud-based EHR software
Healthcare practitioners often host cloud-based EHR or electronic medical records software on remote servers as cost-effective and custom healthcare software solutions for accessing patient data anywhere.
On-Premise-based
With on-premises healthcare EMR/EHR solutions, healthcare businesses get more distinguished governance over data and information as you establish them locally within your workflow infrastructure. Maintenance and support ultimately become their accountability.
Personal Health Records
PHRs are for patients to assist them in monitoring and assessing their health data, such as prescriptions, appointments, and lab test outcomes.
Must-Have Features of EHR Software
The next step in the bifurcated guide is the basic and advanced healthcare software features that define the EMR and EHR software model. When proceeding with healthcare CRM software development, it is valuable to pre-decide the features of EHR software and have a constructive conversation about them. Such a step begins way before development, as the features distinguish the models and ensure the facilitated functioning of the EMR/EHR system. To comprehend the features of EHR software critically, let us expand on their purpose.
Patient Portal
Patients often interact with doctors and hospitals via the patient portal. Extensive details related to their treatment, medications, and lab tests are stored in the portal and can be accessed by them at any given time. EHR patient portal development reduces the back-and-forth to the hospital, dealing with the administrative staff, and long waiting lines for significant information.
Doctor Portal
Before EHR and EMR systems, doctors used to manually update the information and convey it to the administrative department about the same. However, the doctor portals have transformed conventional functioning and are now based on convenience and ease. All the doctor needs to do is update the new information on the portal and make upcoming data on proceeding treatments visible to everyone.
E-Prescription
The convenience-centric phase began with the emergence of e-prescriptions. These eliminated the need to visit the clinic or hospital and ensured that the updated virtual prescription was available to users. This reduced the definitive paperwork requirement, enabling users and patients to remotely manage their medications.
Document Management
With EMR/EHR software development, you can integrate document management tools that keep the necessary information and documents intact. For instance, even though paperwork is lost, the virtual database stores it for patients and hospitals to review in a protected space.
Data Access Control
The EHR/EMR software systems permit access to an individual with authority to go through the documents, lab tests, and prior medication information. Including such healthcare software features in your HIPAA-compliant EMR software empowers the admin with the access to limit the accessibility based on the discretion a patient and their case requires.
Prescription Management
The prescription management features to store and manage previous prescriptions in case of future emergencies. For instance, prescriptions are available with the healthcare establishment and worked with data privacy in mind. You must include the prescription management features to ensure streamlined data safety.
Clinical Records
Including clinical records in the EHR/EMR software is one decision that ensures the healthcare establishment has all the necessary clinical records updated on the system. These records help the doctors and administration take better care of the patients and provide immense patient care.
Reporting
With the reporting and analytics features, EMR software for hospitals provides updates about its comprehensive functioning. From employee management to patient status, everything is represented with graphs and charts to better represent the data and statistics necessary to make data-driven decisions.
Benefits of EMR/EHR Systems
AI in healthcare has shown a significant uprising, and it is due to this primary reason it benefits the industry. The EMR/EHR system benefits section is divided into three segments that bring forth the perspective of comprehensive aspects. Healthcare business owners drive revenue streams and scale their enterprises while providing patients hassle-free access to medical records. Positioning the possibility of advantages custom EHR software development poses, it is high time you navigate your agenda as well.
| For Business Owners | For Patients | For Hospitals |
| Diverse monetization options | Hassle-free access to medical records | Workflow efficiency |
| Business scalability | Facilitated appointment scheduling | Eliminated paperwork |
| Sustainable advantage in a saturated market | Data privacy and safety | Reduced data error |
| Better decision-making | Faster and accurate diagnoses | Cost optimization |
| Cost savings and revenue optimization | Enhanced care coordination | Smooth doctor-patient interactions |
These benefits of EMR/EHR systems apply to all healthcare practitioners who choose custom EMR/EHR software development services from professional experts. As a decision-maker, you must consider the above advantages and rationalize through your final healthcare-centric judgment.
EMR/EHR Software Development Process
When it comes to end-to-end software development services, a systematic approach becomes imperative. Building EHR software may appear straightforward, but it should have a proper flow. Healthcare practitioners and hospitals planning for healthcare software integration into their systems must follow an EHR software development process that considers HIPAA compliance and produces robust healthcare IT solutions.
Define Your Requirement
Beginning with the custom EHR software development process, you must define your requirements before looking for a medical software development company. Comprehending the needs of patients, doctors, and administrative staff can assist in the process. You must ask questions, understand the issues, find solutions, and build a HIPAA-compliant EMR software plan that works in all aspects.
Hire an EMR/EHR Software Development Company
Once the user behavior and probable issue-resolution approaches are instilled, choosing a healthcare software development company is time. As they possess expertise, they also safeguard your software from data breaches and compliance by following HIPAA guidelines. You must determine the experts who have previously worked with healthcare practitioners and bring forth decades of resourceful experience.
Design and Development
As soon as the company is in place, the next step begins when the designers sit down and work on your EHR/EMR software’s layout and UI/US design. You must always keep the idea of reflecting the brand value through your software. The patients must feel connected with the establishment through the design and stay engaged with their medical requirements. As the design is ready, the further EHR development process begins with the front end, back end, and database. All aspects hold equal value, from healthcare software integration to source code development.
Quality Assurance
As soon as the source code is ready, the quality assurance team comes in and is responsible for ensuring that the EMR and EHR software is error-free. They build test cases and test the EHR/EMR software to produce bug-free, error-free, and maintained software. As soon as the back-and-forth between the developers and testers stops, the software will be sent to you to validate it and further forward it for deployment.
Deployment and Maintenance
The validation and assessment phase winds up and sends the EMR/EHR software to the deployment team. They ensure that the software is ready for use and check all the compliances for the release in the market. Once the release is done, the HIPAA-compliant EMR software requires ongoing maintenance and support to perform well throughout. This can be provided by the same EHR/EMR software development company.
Things to Consider During the Custom EHR/EMR Software Development
Before beginning HIPAA-compliant EMR software and healthcare medical app development, you must consider a few parameters that can be helpful throughout the process. Adhering to regulatory compliance, interoperability, and data migration planning are among them.
EHR Regulatory Compliance
The healthcare-centric EMR/EHR app development must adhere to restrictions and ordinances such as HIPAA in the United States, GDPR in Europe, and other regional norms. Compliance and regulations guarantee that patient data is driven lawfully and ethically, patrolling the patient’s privacy and the healthcare provider from legal repercussions.
EHR Software Interoperability
EHR/EMR software interoperability is significant for persuasive EHR software systems, authorizing them to intercommunicate smoothly with other healthcare systems. This interconnectivity stimulates patient communication across distinct media, enhancing care coordination and efficacy.
Data Migration
EHR/EMR software data migration is an influential contradiction when progressing from legacy systems to a contemporary healthcare software development solution. It involves transmitting patient data, medical narratives, and other imperative information to the replacement system without data misplacement or deterioration. This methodology mandates mindful planning, testing, and confirmation to guarantee that all required information is transferred correctly and accurately.
How Much Does EMR/EHR Software Development Cost?
EMR and EHR software are intricate products, and their development will mandate numerous resources. The moderate period for custom EMR software development is 11–18 months long, half of which is devoured by constructing an MVP. The software development cost can range from $40,000 for a rudimentary EMR system to $250,000 for a progressive one.
The cost of EHR software development is based on multiple factors, such as project intricacies, a new and intelligent technology stack, and system complexity. The location and establishment of the development team are also consequential to the HIPAA-compliant EHR software development cost.
EHR Implementation Cost Breakdown
The cost of EHR implementation varies depending on the organization’s size, the system’s complexity, and specific customization requirements. There are two types of EHR implementation costs: direct and indirect. While staff costs, training fees, and unforeseen expenses like security are examples of indirect costs, direct costs are associated with on-premises or cloud implementation.
Here is a thorough cost of implementing an EHR system:
1. Direct Cost of EHR Systems
Purchasing and licensing are only one aspect of the direct expenses associated with EHR implementation in hospitals. To support the EHR systems set up in different departments, businesses should consider license fees, subscription models, custom or on-premise solutions, and additional modules.
-
License Fees and Subscription Models
Modern EHR licensing structures provide flexible payment options, from monthly subscriptions to perpetual licenses, allowing healthcare organizations to align EHR implementation cost structure with operational budgets.
-
Per-provider vs. Enterprise pricing
The cost of implementing EHR in hospitals also depends on the business type. Choose between scalable per-provider pricing for smaller practices or comprehensive enterprise solutions offering unlimited users and enhanced functionality.
-
Cloud-based vs. On-premise Solutions
Cloud-based systems minimize the upfront cost of EMR implementation while offering scalability, whereas on-premise solutions provide greater control over data management and customization capabilities.
-
Additional Module Costs and Customization Fees
Enhance core EHR software features with specialized modules for specific departments or specialties, while custom features can be developed to match unique workflow requirements.
| Component | Small Practice (1-5 providers) | Mid-sized (6-25 providers) | Large Practice (26+ providers) |
| License fees/subscriptions | $600-$2,500/year | $2,000-$4,000/year | Custom enterprise pricing |
| Cloud-based solution | $100-$250/month | $200-$400/month | $300-$600/month |
| On-premise solution | $20,000-$50,000 one-time | $50,000-$100,000 one-time | $200,000+ one-time |
| Additional modules | $1,000-$2,500/module | $2,500-$7,500/module | $7,500-$25,000/module |
2. Hardware and Infrastructure Requirements
Essential technical components and infrastructure upgrades form a substantial portion of electronic medical records software costs, ensuring robust system performance and reliable healthcare delivery.
-
Server and Storage Systems
Robust server architecture and scalable storage solutions to ensure seamless EHR software integration, maintaining quick access to patient data and system reliability.
-
Workstations and Mobile Devices
Ergonomic workstations and secure EHR mobile application integration across all care delivery points, enabling healthcare providers to access patient information whenever and wherever needed.
-
Network Infrastructure upgrades
Network capabilities with high-speed connectivity, redundant systems, and advanced security protocols to support real-time data access increase the cost of electronic health records.
-
Security and Backup Systems
Comprehensive security services for EHR includes encryption, access controls, and automated backup solutions to protect patient data and maintain HIPAA compliance standards.
| Component | Small Practice | Mid-sized | Large Practice |
| Servers/Storage | $2,500-$10,000 | $10,000-$50,000 | $50,000-$250,000 |
| Workstations | $500-$1,000/station | $500-$1,000/station | $500-$1,000/station |
| Network upgrades | $2,500-$7,500 | $7,500-$25,000 | $25,000-$100,000 |
| Security systems | $5,000-$10,000 | $10,000-$37,500 | $37,500-$150,000 |
3. Training and Personnel Costs
Investment in staff training and additional personnel represents a significant portion of EHR implementation cost breakdown, directly impacting long-term adoption success.
Initial Staff Training Programs
Training programs covering system navigation, documentation practices, and workflow optimization ensure a smooth transition and maximize the cost benefits of EHR adoption.
Ongoing Education Requirements
Regular training sessions and updates keep staff proficient with system enhancements, ensuring continued EHR data migration process and high-quality patient care.
Additional IT Staff Hiring Needs
Expand IT team capabilities to support the EHR implementation process, including system administrators, trainers, and technical support specialists for ongoing maintenance.
| Component | Small Practice | Mid-sized | Large Practice |
| Initial training | $1,200-$3,000 | $3,000-$12,000 | $12,000-$60,000 |
| Ongoing education | $600-$1,800/year | $1,800-$6,000/year | $6,000-$30,000/year |
| Additional IT staff | $36,000-$48,000/year | $48,000-$150,000/year | $150,000-$300,000/year |
4. Customization and EHR Integration Costs
EHR systems meet specific organizational needs and connect with existing healthcare platforms, which requires careful planning and substantial EHR implementation cost monitoring.
Custom EHR System for Specific Needs
Custom EHR interfaces, templates, and workflows help match specific organizational needs, optimizing efficiency while maintaining compliance with healthcare documentation.
Integrating with existing systems
Seamlessly connect patient portal integration with EHR, from billing platforms to diagnostic equipment, to create a unified ecosystem for efficient information exchange.
Essential Customization Cost of Implementing EHR
| Customization Type | Small Practice | Mid-sized Practice | Large Practice/Hospital |
| Template Creation | $300 – $900 | $900 – $2,000 | $2,000 – $9,000 |
| Custom Forms | $120 – $480/form | $480 – $600/form | $600 – $1,500/form |
| Specialty-Specific Features | $1,200 – $3,000 | $3,000 – $9,000 | $9,000 – $20,000 |
| Report Customization | $180 – $480/report | $480 – $1,200/report | $1,200 – $2,400/report |
Integration Cost of EHR Implementation
| Integration Type | Small Practice | Mid-sized Practice | Large Practice/Hospital |
| Lab System Integration | $1,200 – $3,000 | $3,000 – $6,000 | $6,000 – $15,000 |
| Medical Device Integration | $900 – $1,800/device | $1,800 – $3,600/device | $3,600 – $7,200/device |
| Billing System | $1,800 – $4,800 | $4,800 – $9,000 | $9,000 – $18,000 |
| Patient Portal | $1,500 – $3,000 | $3,000 – $6,000 | $7,200 – $15,000 |
| E-Prescribing | $600 – $1,500 | $1,500 – $3,000 | $3,000 – $7,000 |
5. Compliance and EHR Maintenance Cost
Ongoing expenses for maintaining regulatory compliance and system upkeep are crucial to the total cost of custom EHR software implementation.
HIPAA-Compliance EHR Implementation Cost
Comprehensive HIPAA-compliant security protocols include access controls, audit trails, and encryption measures to protect patient data and maintain regulatory compliance standards.
Security-based Implementation Cost of Electronic Health Records
Invest in advanced security infrastructure, including multi-factor authentication, endpoint protection, and secure communication channels to safeguard sensitive healthcare information and prevent breaches.
| Component | Small Practice | Mid-sized | Large Practice |
| HIPAA compliance | $3,000-$9,000/year | $9,000-$25,000/year | $25,000-$100,000/year |
| Security measures | $6,000-$15,000/year | $15,000-$40,000/year | $40,000-$180,000/year |
| Annual maintenance | $6,000-$18,000/year | $18,000-$50,000/year | $50,000-$200,000/yea |
| Technical support | $7,200-$14,400/year | $14,400-$35,000/year | $35,000-$100,000/year |
Hidden EHR Implementation Cost and Often-Overlooked Expenses
We all budget for EHR implementation, but what about the hidden costs? From data migration and interface development to data cleaning, let’s uncover the expenses that can impact your bottom line and EHR implementation strategies more than you expect.
Legacy System Data Transfer
Migrating historical patient records, clinical documentation, and administrative data from legacy systems while maintaining data integrity and complete accessibility will ensure substantial costs.
Interface Development with Existing Systems
Interface development between your EHR and existing healthcare solutions comes under EHR implementation hidden costs. However, it enables real-time data exchange while maintaining workflow efficiency.
Data Cleaning and Standardization
One of the EHR implementation cost factors includes data cleaning. Inconsistent legacy data in standardized formats ensure accuracy and usability while meeting current healthcare documentation requirements.
| Component | Small Practice | Mid-sized | Large Practice |
| Data migration | $3,000-$9,000 | $9,000-$25,000 | $25,000-$100,000 |
| Interface development | $1,200-$3,000/interface | $3,000-$7,000/interface | $7,000-$20,000/interface |
| Data cleaning | $1,800-$6,000 | $6,000-$12,000 | $12,000-$60,000 |
Segmenting the Cost of Implementing EHR by Facility Type
Earlier, we talked about the hidden costs of EHR implementation. Now, let’s dive deeper and break it down by facility type. Whether you’re running a small clinic, a specialty center, or a large hospital, understanding these cost variations will help you budget smarter and make informed decisions.
EHR Implementation Costs for Solo/Small Practice (1-3 providers)
| Cost Category | Initial Investment | Annual Recurring Costs |
| Software Licensing | $8,000 – $16,000 | $2,400 – $4,500/provider |
| Hardware | $1,500 – $3,000/provider | $300 – $600/provider |
| Training | $1,800 – $3,000 | $600 – $1,200 |
| Implementation Services | $3,000 – $6,000 | N/A |
| Maintenance & Support | N/A | $1,400 – $2,800/year |
| Total Range | $15,000 – $30,000 | $4,700 – $9,100/year |
EHR Implementation Cost Breakdown For Mid-sized Clinical Practice (4–10 providers)
| Cost Category | Initial Investment | Annual Recurring Costs |
| Software Licensing | $24,000−$51,000 | $2,100−$4,200/provider |
| Hardware | $15,000−$30,000 | $3,000−$6,000 |
| Training | $6,000−$12,000 | $1,800−$3,600 |
| Implementation Services | $9,000−$18,000 | N/A |
| Maintenance & Support | N/A | $7,200−$14,400/year |
| Total Range | $54,000−$111,000 | $20,400−$66,000/year |
Cost of Implementing an EHR System for Small Hospitals (Under 100 beds)
| Cost Category | Initial Investment | Annual Recurring Costs |
| Software Licensing | $50,000−$100,000 | $20,000−$30,000 |
| Hardware | $40,000−$150,000 | $15,000−$25,000 |
| Training | $30,000−$60,000 | $7,000−$14,000 |
| Implementation Services | $45,000−$90,000 | N/A |
| Maintenance & Support | N/A | $15,000−$30,000/year |
| Total Range | $170,000−$400,000 | $57,000−$99,000/year |
EHR Implementation Costs for Large Hospitals/Health System (500+ beds)
| Cost Category | Initial Investment | Annual Recurring Costs |
| Software Licensing | $60,000-$150,000 | $25,000-$40,000 |
| Hardware | $70,000−$140,000 | $20,000-$35,000 |
| Training | $50,000−$100,000 | $15,000-$30,000 |
| Implementation Services | $60,000−$120,000 | N/A |
| Maintenance & Support | N/A | $20,000-$40,000/year |
| Total Range | $240,000−$510,000 | $80,000−$145,000/year |
Cost of Implementing EHR For Specialty Facilities
| Facility Type | Initial Investment | Annual Recurring Costs |
| Ambulatory Surgery Center | $120,000−$240,000 | $24,000−$48,000 |
| Urgent Care Center | $45,000−$90,000 | $9,000−$18,000 |
| Mental Health Facility | $60,000−$150,000 | $12,000−$30,000 |
| Rehabilitation Center | $90,000−$180,000 | $18,000−$36,000 |
| Long-term Care Facility | $150,000−$300,000 | $30,000−$60,000 |
How Much EHR Implementation Costs: Final Pricing
The average cost of EHR implementation varies significantly based on facility size and requirements, ranging from $15,000 for solo practices to over $510,000 for large hospitals. Understanding these price ranges helps organizations budget effectively for digital transformation.
| Facility Type | Total First-Year Cost | Annual Recurring Cost |
| Solo Practice (1-3 providers) | $15,000 – $30,000 | $4,700 – $9,100/year |
| Small Practice (4-10 providers) | $54,000−$111,000 | $20,400−$66,000/year |
| Small Hospital (<100 beds) | $170,000−$400,000 | $57,000−$99,000/year |
| Large Hospital (500+ beds) | $240,000−$510,000 | $80,000−$145,000/year |
*Note: These approximate costs can vary significantly based on location, specific vendor selection, existing infrastructure, and unique organizational requirements.
Also Read | Healthcare App Development Cost in 2025
Costs of Popular EHRs
EHR software costs vary, and various expenses are associated with implementation. Everyone asks how much epic EHR implementation costs for small practices. Due to its popularity, Epic is one of numerous EHR choices, including off-the-shelf and customizable ones.
The cost of EHR systems differs based on several aspects, like practice size and specialty. 96% of practices employ any sort of EHR software, whereas specialists generally want additional functionality and customization, resulting in more significant expenditures.
Although they may have recurring subscription costs, cloud-based solutions are usually less expensive upfront than on-premise systems. The feature sets and price structures of various providers vary. Here is a broad summary of the prices of various well-known EHRs, though.
| EHR System | Pricing Model | Cost per User/Month as of 2024 |
| Epic | Subscription | $200 (for basic features) and $35,000 (for advanced features) |
| Athenahealth | Subscription | $140 |
| eClinical | Subscription | $449-$599 |
| Meditech | Perpetual license or subscription | $49 |
| Cerner | Subscription | $25 |
Challenges and Solutions Impacting the Cost of EHR Implementation
Healthcare organizations face various challenges in EHR implementation that can significantly impact costs, but strategic solutions can help minimize these financial obstacles.
1. Staff Resistance to New Technology
Resistance to change leads to delayed adoption and extended training periods, increasing operational costs and reducing productivity.
Solution
Implement early change management programs and peer champion initiatives, offering incentives for quick EHR impact on patient care while providing comprehensive support during the transition period.
2. Data Migration Complexities from Legacy Systems
It can cause unexpected EHR implementation costs through extended timelines, additional resource requirements, and potential data integrity issues.
Solution
Deploy automated data migration tools and dedicated migration teams while conducting thorough pre-migration analysis to identify and address potential issues early.
3. Insufficient Hardware Infrastructure
Unexpected upgrades to network systems, servers, and workstations led to significant unplanned capital expenditure.
Solution
Conduct a thorough infrastructure assessment before EHR implementation, creating a phased upgrade plan that aligns with budgetary constraints and operational requirements.
4. Integration Difficulties with Existing Healthcare Systems
It can cause workflow disruptions and require additional custom development work to ensure compatibility.
Solution
Prioritize EHR vendors by offering robust API capabilities and pre-built integrations while developing a detailed integration roadmap before implementation begins.
Why Choose SparxIT as Your Trusted EMR/EHR Software Development Company?
At SparxIT, we have a demonstrated record of cogitating and engineering EHR for both hospital and patient-facing. Our team of expert developers, with their in-depth acquaintance of healthcare compliance, guarantees the composition of efficacious EHR software that complies with all regulations like HIPAA, GDPR, and many more.
This, along with our healthcare development team’s invaluable insight into future-ready HIPAA-compliant EMR software, makes us a dependable leader in the healthcare software space. We combine an exemplary combination of dexterity and technology comprehension to assist you in constructing and executing an efficient EHR in your healthcare system. Contact to find out the exact EMR software development cost that fits your needs.

Partner with Experts
Frequently Asked Questions
Why should my healthcare business invest in EHR software solutions?









EHR software development streamlines workflows, improve patient care, and ensure compliance. They enhance data accessibility, reduce errors, and boost operational efficiency, making them a wise long-term investment.
What are the benefits of partnering with an EHR software development company?
















Benefits include access to custom, scalable, and secure EHR solutions. Additionally, EHR software ensures compliance, interoperability, and improved patient care while reducing development time and costs.
What are the key factors affecting EHR implementation costs?
















The cost of EHR implementation depends on system type (cloud vs. on-premise), customization, training, hardware, data migration, and ongoing maintenance. Each factor impacts the overall budget significantly.
How much does EMR software development cost?
















The cost of EMR software development varies based on features, customization, and compliance needs. Generally, basic software costs from $30,000 to $150,000. However, a more advanced HIPAA-compliant and AI-powered solution can range from $50,000 to $350,000.
What are the common challenges in EHR implementation?
















Common challenges in integrating EHR include staff resistance, data migration issues, workflow disruptions, high costs, and ensuring compliance. Proper planning and training can mitigate these hurdles.
How to calculate the ROI of EHR implementation?
















Calculate ROI by comparing savings from reduced paperwork, improved efficiency, and fewer errors against implementation and maintenance costs. Track measurable outcomes like patient satisfaction.
How to reduce the cost of EHR implementation?
















Opt for cloud-based solutions, prioritize essential features, negotiate vendor pricing, and invest in staff training to minimize disruptions and avoid costly mistakes during implementation.




